Influenza like illness
This year’s flu season continues to accelerate. CDC released data yesterday showing that 5.5% of visits to outpatient providers were for influenza like illness (ILI), a term that includes complaints of fever and cough or sore throat. The current trajectory puts this season on track to be one of the worst in the last decade, and well ahead of the usual winter timeline.
Although ILI captures more viruses than just influenza, it’s clear that influenza has made a big comeback this year after several seasons of quiet. CDC estimates that there have already been 23,000 hospitalizations and 1,300 deaths from flu, including five pediatric deaths (+3 this week). H3N2 and H1N1 are the dominant strains so far. Both are included in the 2022-2023 flu vaccine so I’m hoping it’s a good match this year, though the agency’s website does warn that flu vaccines are typically less effective against H3N2.
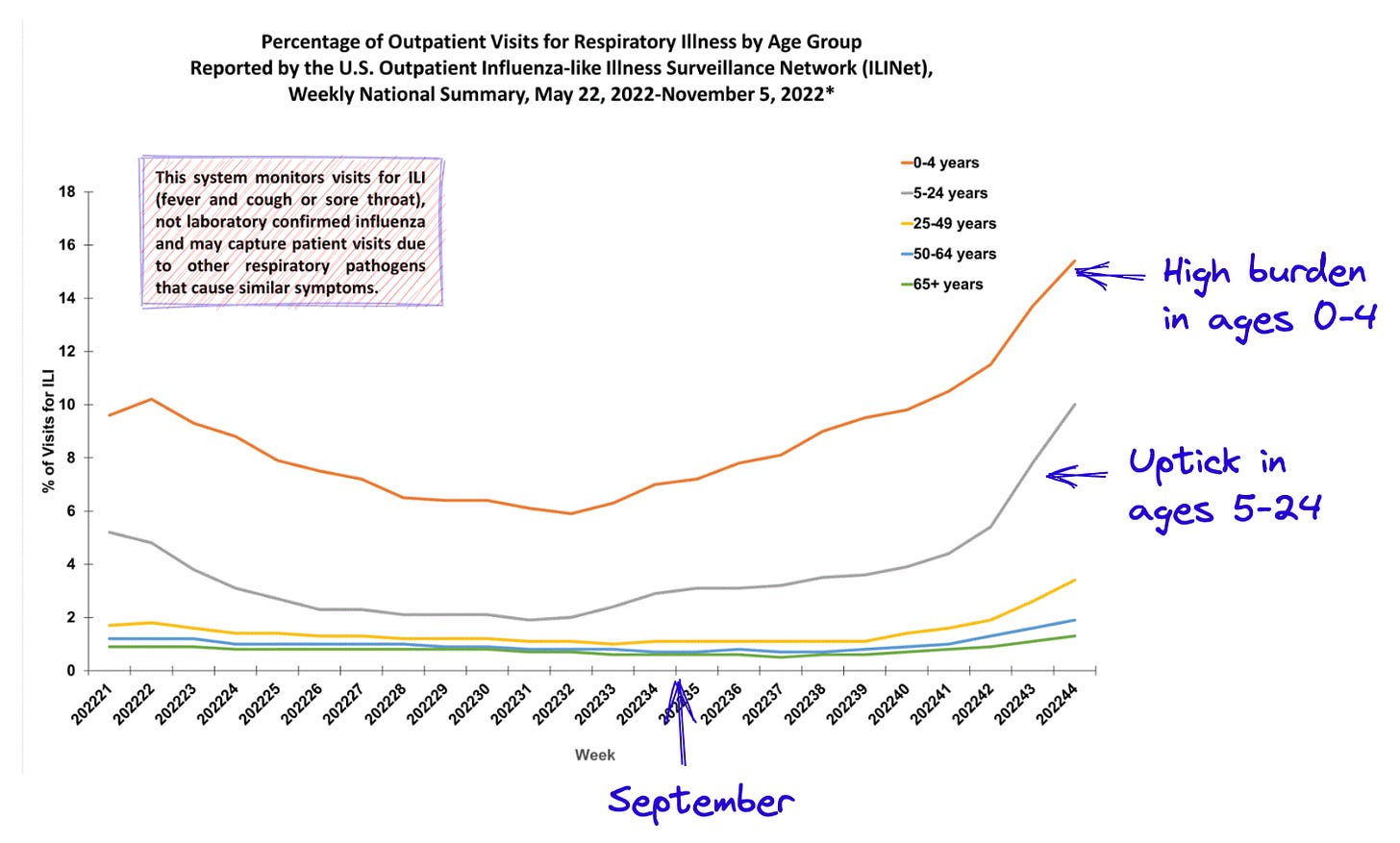
This week, I’ve annotated the charts below to aid in interpretation. Epidemiology uses week of the year rather than dates to mark time, so I’ve also added markers to clarify timeline.

As in past weeks, young children are the hardest hit by ILI. The percentage of outpatient visits for kids under 4 has now hit 15%, meaning 1 in 7 visits to the doctor are for ILI in that age group. School age children and young adults (ages 5-24) have also seen a marked increase in recent weeks. These trends are driven in part by a surge of RSV, which is highest it has been since at least 2018. Although RSV can affect people of any age, it is most dangerous in young children and older adults.
I don’t really see signs of slowing in the RSV data, but it’s less well surveilled than flu so it’s difficult to make reliable, real-time assessments.
Twenty five jurisdictions have high or very high levels of ILI activity, up from nineteen last week. The southeast, south-central and mid-Atlantic regions are most heavily affected, but as I said last week, I wouldn't take comfort if you live in a “green” state. I expect the season to get worse before it gets better. Please get your flu shot if you haven’t already, wash your hands frequently, and consider wearing a high-quality mask.

Covid-19
Last week, I wondered whether the U.S. may be headed into another covid-19 wave. This week, I see more evidence for this scenario. Cases and hospitalizations have begun to tick up, as has test positivity. Fourteen states and Washington D.C. have seen a double-digit rise in hospitalizations over the last two weeks. The rise is most evident in hospitalization rates in older adults, the group that is most vulnerable to developing severe disease. Unfortunately, just 27% of adults 65 and older have received an updated bivalent booster, which I worry will contribute to an increase in hospitalizations.
It’s too soon to say we’ll see another wave for sure, but coupled with the early and widespread flu season, the healthcare system is likely facing another difficult winter season.

As an aside, I am often asked why I continue to look at case counts even though the widespread use of home testing (the results of which are not reported to public health authorities) has made it a less reliable indicator. While I agree that this is the case, I still find case counts to be a useful and early indicator of changing trends. I look at them in conjunction with data on hospitalizations, testing, and wastewater to get a complete picture of how things are changing.
Monkeypox
Happily, the monkeypox epidemic in the United States continues to steadily decline. The average number of daily new cases nationwide is now below 30, down from a high of around 450 in August. The effective reproduction number remains well below 1, which is further evidence that the outbreak is shrinking.

I’m hoping we get estimates of the effectiveness of Jynneos, the vaccine used to prevent monkeypox, soon. I have not seen any new data since CDC released a preliminary analysis in late September. That analysis does not fully account for the dose-sparing strategy that was implemented in August, and it also does not evaluate whether the vaccine’s ability to protect against infection wanes over time.
Gathering this kind of data is often difficult in an outbreak setting. As the number of new cases declines over time, fewer people who received the vaccine are exposed and infected so there is no way to evaluate how well the vaccine works. Although the decline in incidence is roundly good news for public health, it does leave open questions that can be frustrating when the next outbreak pops up.
Reader poll
I want to know more about what Force of Infection readers are interested in. What kind of content would you like to see more of:
News you can use. Updates on flu season, COVID-19, and other infections that impact a huge number of daily lives. Example.
Emerging infectious diseases. Updates on outbreaks of emerging or re-emerging infectious diseases around the globe, like Ebola virus disease, hantavirus, monkeypox, etc. Example.
Deeper dives. A closer look for people who already follow epidemiology topics extensively. Example.





Unusual ILI was what keyed me into the pandemic potential on 18 JAN 2020, when I pivoted from chairing a session at a meteorology conference to looking at the issue that'd been in the news for a couple of weeks. I was able to glean enough data on the flight home to decide, at least for myself, that we were in for a wild ride. And that SARS-CoV-2 was likely already in the US. I really need to go back and resurrect the notes from the old laptop (since somewhat dead) I used on that flight.
Thanks. Color it done. And thank you for the annotations. Saved me from having to create (or reinvent) the material again.